General aspects of POP
Pelvic Organ Prolapse (POP) is a condition in women, where one or more of the pelvic organs is bulging or descending into or through the vagina.The wordprolapse comes from the Latin prolabi, which means "falling" or "slipping". Organs from 3 different compartments can be part of POP: the anterior compartment with the bladder in front, the middle compartment with the uterus or vaginal top(if there is no longer a uterus) and the posterior compartment, with the (large) intestine located behind it.
There is no clearly defined cause of POP and there is no simple uniform treatment of POP leading toan ongoing lively debate about both treatmentand prevention of a prolapse.
POP is a common worldwide health problem and can be a significant burden for the individual woman as well as for the society. Although POP does not often lead to serious illness or death, it does cause a lot of complaints, so that the quality of life of women with a POP is greatly affected.30
Anatomical aspects
The bottom of the abdominal cavity is closed by the pelvic floor. The pelvic floor consists of a system of muscles and connective tissue and ensures that the urine, stool and a fetus cannot just leave the body. In addition, organs such as the bladder, rectum and uterus remain in place. The anatomical support of the organs of the small pelvis is provided by the musculus levator ani complex as well as by the connective tissue complex in the small pelvis. For example, the uterus is held in place by several ligaments of which the sacro-uterine ligament (from cervix to sacrum) is an important pillar. The position of the vagina (the direction of the vaginal axis) also plays a role in the anatomical support: an almost horizontal position of the vagina acts as a valve when the abdominal pressure is increased. Proper nerve provision is necessary for a properly functioning pelvic floor. Dysruption or dysfunction of one or more components of this pelvic floor complex leads to reduction of support and ultimately to prolapse of pelvic organs.1
Symptoms
Women who seek helpbecause of POP can have a range of complaints.2The most specific complaint is seeing or feeling a bulge. In addition, complaints can occur with regard to the bladder function: incontinence for urine, frequent micturition, incomplete urination, inability to urinate, position change necessaryto urinate. Complaints with regard to bowel function are: incontinence for flatus, fluid or faeces; pain, digital help needed for evacuation of urine or faeces. Sexual dysfunction can also be a consequence of a POP.
Although POP is one of the most common indications for a gynaecological operation, there are relatively few studies on incidence and prevalence of POP.3 A prevalence of symptomatic POP between 4-12% of all women has been reported for Australia and Sweden.4,5One of the few population studies shows that about 40% of women have a stage 2 or more prolapse.6 The probability that a prolapse causes serious discomfort is much lower (11%). A large US study shows a prevalence of 14.2% in all women, resp 41% for women between 50-79 years of age.7
A review of studies in developing countries demonstrates a higher mean prevalence of of POP 19.7% in these countries.8As studies have major differences in design, definitions and methods, the value of comparison of results is limited. In a systematic review is stated that the low and lower income countries have almost twice the burden of POP than countries of the higher economy.28 Future POP incidence, prevalence, and natural history studies should include non-white women from LMICs and should combine pelvic examination data with validated patient-reported outcome measures when feasible. Anticipated future service needs differ globally, with a greater demand for POP treatment services in well-resourced settings where aging populations are prevalent.37
A physical examination is the cornerstone for diagnosing POP and for assessing the type and severity of anatomical abnormalities. The examination is usually done in a lithotomy position; both the abdomen and the pelvis are examined externally and internally. The examination is done at rest and at maximum press (Valsalva); all 3 compartments (anterior, middle and posterior) are assessed separately. Also, the overall muscle strength and coordination of the pelvic floor muscles are assessed.
Examination in standing position can be useful if there is a discrepancy between the complaints of the woman and the findings in the research in lithotomy position.2
The place of urodynamic testing is under debate; so far there is no evidence that preoperative urodynamic investigation improves the outcome of prolapse surgery.
The severity of a prolapse use can be quantified in 4 stages with the Pelvic Organ Prolapse Quantification (POP-Q) score.9 In this POP-Q system 9 anatomical landmarks are measured in centimetres to quantify abnormalities, see fig 1. The POP-Q score succeeded previously used scoring systems, see fig 2. It has a good inter-observer agreement and is also suitable for objectifying changes after surgery.Various radiographic modalities have been proposed to measure the extent of POP like for example Dynamic Magnetic Resonance Imaging (MRI, transperineal ultrasound and 3-4D ultrasound have been used in staging POP, but so far all these techniques do not appear to be superior to clinical assessment of POP.10
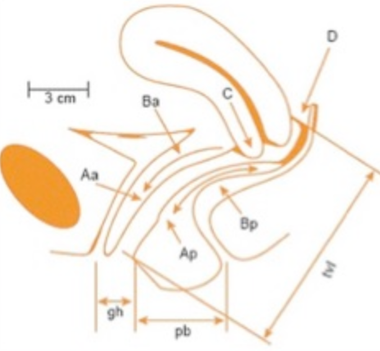
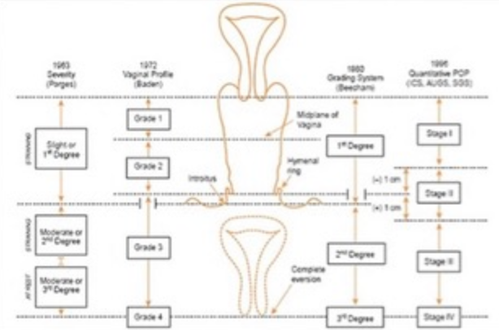
fig 1 POP-Q scoring system fig 2 POP scoring systems
The development of a prolapse has been determined to be multi-factorial. The factors that contribute to the development of a prolapse can be divided into established risk factors and potential risk factors.
Vaginal childbirth is the factor most frequently associated with prolapse and also advancing age and obesity are established risk factors.2 Childbirth can lead to muscular and neurological damage. Poor levator muscle function might be the first step in a process that ultimately causes failure of the connective tissue supports of the pelvic organs.1,11 In a substantial minority of women delivering vaginally, the puborectalis muscle is shorn off the pelvic side wall. This avulsion risk is strongly associated with age at first delivery and vaginal operative delivery.3
Potential risk factors for developing a POP are: pregnancy, prolonged second stage of labour, high birthweight child, shape of pelvis, hysterectomy,13 family history positive for POP14, race or ethnic origin, connective tissue disorders and chronic predisposing factors like heavy lifting, constipation and coughing.25
Reduction of obstetric risk factors offers the potential to prevent subsequent POP. But until now, there is a lack of evidence in this area. Some researchers have mentioned elective caesarean section as a way to reduce risk of POP. However, until specific selection criteria allow providers to ascertain who would and would not benefit from this intervention, it is unlikely to become an effective strategy for prevention.2Some evidence is available for lifestyle changes like reduction of weight in case of obesity. In an experimental and prospective study there is some indication that strenuous exercise increased POP symptoms and reduced pelvic floor support.35 There is also increasing attention for preventive surgery in case of hysterectomy for non-POP indications.31
Expectant management
Many women with POP, especially those with minor degrees of prolapse not extending the hymenal remnants, complain of little or no discomfort. In such cases a policy of expectant management is appropriate. Weight reduction and lifestyle adjustment can be useful if relevant.2
Pelvic floor muscle training
Although studies have been published on the effectiveness of pelvic floor muscle training in the treatment of genital prolapse, established scientific evidence on the value of physiotherapy is lacking. The conclusions of published studies suggest a short-term positive effect on the experience of the severity of the complaints without a positive effect on the anatomical abnormality itself. A recent study shows a statistical significant improvement in symptoms, but the difference between the studied groups was not clinically relevant.15 For the time being, the role of pelvic floor muscle training in patients with a prolapse is mainly beneficial for the treatment of micturition, defecation and sexual complaints.
Pessary treatment
From ancient times mechanical devices have been used to reposition prolapsed organs.Pessaries offer a safe, non-surgical option for the treatment of POP.29 Especially in lower grade POP cases the use of a pessary may result in decreasing the frequency and severity of prolapse symptoms and may avert or delay the need for surgery.16,17 Pessary use can prevent worsening of the prolapse.18 A recent study in patients with symptomatic POP has shown that nearly two-thirds of women choose a pessary rather than surgery as initial management.19 The preference for pessary treatment over surgery appears not to be influenced by differences in POP symptoms like bowel or sexual function.
Complications associated with pessary insertion and use include vaginal discharge, ulcerations, excoriations, bleeding, pain, urinary and/or faecal impaction and pessary expulsion.20 Rarely, pessaries cause major urinary, rectal or genital complications such as fistula, hydronephrosis and urosepsis.2 These complications are almost exclusively related to a long period of use or neglected use.26
Although traditionally thought of a treatment only for women deemed unfit for surgery or infirm, pessaries are a viable treatment option for the majority of women in the initial management of POP.
Pessary fitting is achieved through trial and error. Correct fitting relieves patient symptoms, allows the patient to void and defecate, stays in place with activity and causes no discomfort to the patient.27 Not in all women/cases a pessary can be inserted or continued for a longer period. In a prospective study 74% of women with symptomatic POP had a pessary fitted successfully.21 Success rates, defined as continued pessary use in women who have a pessary fitted, range from 56 to 89% at 2–3 months21,22, and 28% at 5 years months after insertion.23 Risk factors for pessary failure are: previous hysterectomy, increased parity, a short vaginal length and wide vaginal introitus, which can occur after prolapse surgery and hysterectomy.
Pessary treatment can be offered to woman by health care workers with very limited resources, important for remote areas of low-income countries.
Followup visits involve removal and cleaning of the pessary, inspection of the vaginal wall and afterwards replacing the pessary. Intervals between these follow up visits vary widely and studies about the ideal length of such intervals are lacking.32,33
Vaginal pessaries can be broadly divided into two types: support and space-filling pessaries. As there is no evidence to support the use of a specific type of pessary, choice can be based on experience and costs. It is generally accepted that the ring pessary should be the first choice because of ease of insertion and removal. Folding the pessary reduces its size and allows for easy introduction through the vaginal introitus. Its shape prevents collection of vaginal discharge and women can continue to engage in vaginal intercourse with the pessary in situ. The ring pessary with supportmembrane, is useful in cases of procidentia as the uterus cannot prolapse through the closed ring. If the ring pessary fails, other pessaries can be used. Currently, the pessaries are made of silicone or polyvinyl.
Surgical treatment and pessary treatment are both efficacious in reducing the presence and severity of prolapse symtoms.34 Women with symptomatic POP who decline pessary treatment or when such treatment fails, require surgical intervention.The risk for a woman to undergo surgery in her life due to a prolapse is 11-19%.24
Surgical treatment for POP can be categorised into reconstructive and obliterative procedures.
Reconstructive surgery aims to correct the prolapse while maintaining vaginal sexual function and relieving any associated pelvic symptoms.3Surgery is not 100% successful. New or recurrent prolapses will occur in a significant percentage (up to 30-35%) and these can be difficult to repair.24
Options for reconstructive surgical repair of POP can be classified by compartment and can be subdivided into abdominal and vaginal procedures.
For a prolapse of the anterior compartment the most used procedure is a colporrhaphia anterior (or possibly variants), for the posterior compartment a colporrhaphia posterior (or possibly variants). These operations, depending on the anatomical outcome measure used, give a considerable chance of recurrences, which are regularly asymptomatic.
As far as symptomatic prolapse of the middle compartment is concerned, the vaginal hysterectomy, whether or not with shortening and suturing of the sacrouterine ligaments in the vaginal top, has been the preferred treatment for some time. However, there has been increasing interest in uterine-saving surgery in recent years. This is because it is becoming clear that not the uterus itself is the cause of the prolapse but the lack of suspension: especially the suspension system of the uterus was found to be inadequate. Various old and new alternative methods receive more attention, such as the sacrospinal hysteropexy and the (modified) Manchester operation.36
Obliterative surgical procedures may be suitable for women who do not wish to preserve coital function. Colpocleisis corrects POP by moving pelvic viscera back into the pelvis and closing off the vaginal canal partly or totally. This type of surgery is associated with high cure rates (up to 95%), fast recovery times and less complications.2,3
The rationale for using implants in prolapse surgery is that an implant replaces deficient body's own material, gives reinforcement provided by increasing the support surface and induces new support tissue. Although in the short-term operations with vaginal mesh result in better anatomical and functional outcome, the risk of (long term) complications is the reason that operations with mesh are reserved for women with recurrent prolapse.
1. The scientific basis of prolapse. Hughes P, Jackson SR. The Obstetrician & Gynaecologist. July 2000: 2 no 3.
2. Pelvic organ prolapse - a review. Dietz HP. Aust Fam Physician. 2015. Jul;44(7):446-52
3. Pelvic organ Prolapse. Jelovsek JE, Maher C, Barber MD.www.thelancet.com. Vol 369 March 24, 2007
4. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. Maclennan AH, Taylor, AW, Wilson DH, Wilcon D. Br J Obstet Gynaecol. 2000 Dec;107(12):1460-70.
5. Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Tegerstedt G, Maehle-Schmidt M, Nyrén C, Hammarström M. Int Urogynecol J Plevic Floor Dysfubct. 2005 16(6):497-503
6. Symptomatic pelvic organ prolapse and possible risk factors in a general population.Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, Steegers-Theunissen RP, Burger CW, Vierhout ME.Am J Obst Gyn. 2009 Feb;200(2):184.e1-7. doi: 0.1016/j.ajog.2008.08.070. Epub 2008 Dec 25.
7. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Am J Obstet Gynecol. 2002 Jun;186(6):1160-6.
8. Pelvic Organ prolapse and incontinence in developing countries; review of prevalence and risk factors. Walker GJA, Gunasekera P. Int Urogynecol J 201 1;22:127-35
9. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. Am J Obstet Gynecol. 1996;175:10-7.
10. Pelvic organ prolapse symptoms in relation tot POPQ, ordinal stages and ultrasound prolapse assessment. Kluivers KB, Hendriks JC, Shek C, Dietz HP. Urogynecology Journal and Pelvic Floor Dysfunction 19: 1299-1302.
11. The natural history of pelvic organ support in pregnancy. O'Boyle AL, O'Boyle JD, Ricks RE, Patience TH, Calhoun B, Davis G. Int Urogynecol J Pelvic Floor Dysfunct. 2003 Feb;14(1):46-9; discussion 49.
12. The aetiology of prolapse. Dietz HP. Int Urogynecol J (2008) 19:1323-1329.
13. Epidemiology of genital prolapse: observations from the Oxford Family Planning Ass Study. Mant J, Painter R, Vessey M. Br J Obstet Gynaecol. 1997 May;104(5):579-85.
14. A systematic review of clinical studies. 24 on hereditary factors in pelvic organ prolapse.Lince SL, van Kempen LC, Vierhout ME, Kluivers KB.Int Urogynecol J. 2012;23(10):1327-36.
15. International urogynecology consultation chapter 3 committee 2; conservative treatment of patient with pelvic organ prolapse: Pelvic floor muscle training. Bø K, Anglès-Acedo S, Batra A, Hoff Braekken I, Chan YL, Homsi Jorge C, Kruger J, Yadav M, Dumoulin C. Int Urogynecol J. 2022;33:2633-2667
16. Nonsurgical management of pelvic organ prolapse. Culligan PJ. Clinical Expert series Vol 119, no 4. April 2012.
17.Pessaries (mechanical devices) for managing pelvic organ prolapse in women (Review).Bugge C, Adams EJ, Gopinath D, Stewart F, Dembinsky M, Sobiesuo P, Kearney R.Cochrane Database of Systematic Reviews2020, Issue 11. Art. No.: CD004010. DOI:10.1002/14651858.CD004010.pub4.
18. Do pessaries prevent the progression of pelvic organ prolapse? Handa VL, Jones M. Int Urogynecol J Pelvic Floor Dysfunct 2002;13:349-51.
19. Prospective evaluation of outcome of vaginal pessaries versus surgery in women with symptomatic pelvic organ prolapse. Abdool Z, Thakar R, Sultan AH, Oliver RS. Int Urogynecol J Pelvic Floor Dysfunct 2010;22:273-8.
20. Pessary treatment for pelvic organ prolapse and health related quality of life: a review. Lamers BHC, Broekman BMW, Milani AL. Int Urogynecol J 2011 22:637-644
21. A simplified protocol for pessary management. Wu V, Farrell SA, Baskett TF, Flowerdew G. Obstet Gynecol 1997;90:990-4.
22. Patient characteristics that are associated with continued pessary use versus surgery after 1 year. Clemons JL, Aguilar VC, Sokol ER, Jackson ND, Myers DL. Am J Obstet Gynecol 2004;191:159-64.
23. A 5-year prospective study of vaginal pessary use for pelvic organ prolapse. Lone F, Thakar R, Sultan AH, Karamalis G. Int J of Gynaecology and Obstetrics 2011 114:56-59
24.Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL.Obstet Gynecol. 1997 Apr;89(4):501-6.
25. Pelvic floor function is independently associated with pelvic organ prolapse, Brækken IH, Majida M, Ellström Engh M, Holme IM, Bø K. BJOG 2009;116:1706-1714
26. Management of the neglected vaginal ring pessaries. Fernando RJ, Sultan AH, Thakar R, Jeyanthan K. Int Urogynecol J (2007) 18: 117-119
27. Vaginal pessaries in managing women with pelvic organ prolapse and urinary incontinence: patient characteristics and factors contributing to success. Hanson LAM, Schulz JA, Flood CG, Cooley B, Tam F. Int Urogynecol J (2006) 17: 155-159.
28. Pelvic organ prolapse in counties of different economy: a systematic review. Paudel S, Chalise A. Dangal G, Bhandari TR, Baral G,. Nep J Obstet Gynecol 2019;14(29):7-21
29. The history and usage of vaginal pessary: a review. Oliver R, Thakar R, Sultan AH. Eur J of Obstetrics & Gynecology and Reproductive Biology 156 (2011) 125-130.
30. A qualitative evidence synthesis using meta-ethnographic to understand the experience of living with pelvic organ prolapse. Toye F, Pearl J, Vincent K, Barker K. Int Urogynecology Journal 2020 https://doi.org/10.1007//s00192-020-04494-z
31. The effectiveness of surgical procedures to prevent post-hysterectomy pelvic organ prolapse: a systematic review of the literature. Carlin GL, Bodner-Adler B, Husslein H, Ritter M, Umek W. Int Urogynecology Journal 2021 32:775-783
32. Effect of pessary cleaning and optimal time interval for follow-up: a prospective cohort study. Thys SD, Hakvoort RA, Asseler J, Milani AL, Vollebregt A, Roovers JP. Int Urogynecology Journal 2020 31: 1567-1574
33. Timing of Office-Based Pessary Care. Propst K,Mellen C,O’Sullivan DM,Tulikangas PK.Obstet Gynecol 2020;135:100-5
34. Pessary or surgery for a symptomatic pelvic organ prolapse: the PEOPLE study, a multicentre prospective cohort study. Van der Vaart LR, Vollebregt A, Milani AL, Lagro-Janssen AL, Duijnhoven RG, Roovers JPWR, Van der Vaart CH. BJOG 2022 129(5):820-829
35. Streneous physical activity, exercise, and pelvic organ prolapse: a narrative scoping review. Bó K,Anglès-Acedo S, Batra A, Hoff Braekken I, Chan YL, Homsi Jorge C, Kruger J, Yadav M, Dumoulin C. Int Urogynecol J. https://10,1007/s00192-023-05450-3
36. A comparison of long-term outcome between Manchester Fothergill and vaginal hysterectomy as treatment for uterine descent. Thys SD, Coolen AL, Martens IR, Oosterbaan HP, Roovers, JPWR, Mol BW, Bongers MY. Int J Urogynecol J 2011 22:1171-1178
37. International urogynecology consultation chapter 1 committee 2: Epidemiology of pelvic organ prolapse: prevalence, incidence, natural history, and service needs. Brown HW, Hegde A, Huebner M, Neels H, Barnes HC, Tarquini GV, Mukhtarova N, Mbwele B, Tailor V, Kocjancic E, Trowbridge E, Hayward L. Int Urogynecol J. 2022 33(2):173-187